Abstract
Individuals with hypertension need to stay on therapy with antihypertensive medication to obtain the full benefits of blood pressure reduction. There are important differences in tolerability across antihypertensive drug classes, and these differences influence the extent to which patients are willing to continue taking their drugs. Three separate sources of evidence—postmarket surveillance studies, medical/prescription database studies, and discontinuation of study medication in long-term endpoint clinical trials—support the proposition that angiotensin II antagonists, the newest class of antihypertensives, are well tolerated, and that patients whose initial treatment is an angiotensin II antagonist are more likely to persist with therapy than patients who use other classes of antihypertensives. Recent landmark trials with losartan in hypertensive patients with left ventricular hypertrophy (Losartan Intervention For Endpoint reduction [LIFE]) and in diabetes (Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan [RENAAL]) demonstrated excellent tolerability, a high level of persistence, and clinical benefits exceeding those provided by blood pressure control alone for the prototype angiotensin II antagonist in clinical settings.
Similar content being viewed by others
References and Recommended Reading
American Heart Association: 2002 Heart and Stroke Statistical Update. Dallas: American Heart Association; 2001.
Hodgson TA, Cai L: Medical care expenditures for hypertension, its complications, and its comorbidities. Med Care 2001, 39:599–615.
Joffres MR, Hamet P, MacLean DR, et al.: Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens 2001, 14:1099–1105.
Marques-Vidal P, Ruidavets J-B, Cambou J-P, et al.: Trends in hypertension prevalence and management in Southwestern France, 1985–1996. J Clin Epidemiol 2000, 53:1230–1235.
Banegas JR, Rodríguez-Artalejo F, José de la Cruz Troca J, et al.: Blood pressure in Spain: Distribution, awareness, control, and benefits of a reduction in average pressure. Hypertension 1998, 32:998–1002.
The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1997, 157:2413–2466.
Guidelines Subcommittee: 1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. J Hypertens 1999, 17:151–183.
Payne KA, Esmonde-White S: Observational studies of antihypertensive medication use and compliance: is drug choice a factor in treatment adherence? Curr Hypertens Rep 2000, 2:515–524. This is a very thorough review of the historical literature on factors contributing to antihypertensive medication compliance, and on results of observational studies on adherence to therapy.
Sackett DL, Haynes RB, Gibson FS, et al.: Randomized clinical trial of strategies for improving medication compliance in primary hypertension. Lancet 1975, 1:1205–1207.
Iskedjian M, Einarson TR, MacKeigan LD, et al.: Relationship between daily dosing frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther 2002, 24:302–316.
Choo PW, Rand CS, Inui TS, et al.: Validation of patient records, automated pharmacy records and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care 1999, 37:846–857.
Coons SJ: Medication compliance: the search for answers continue [editorial]. Clin Ther 2001, 23:1294–1295.
Düsing R: Adverse events, compliance, and changes in therapy. Curr Hypertens Rep 2001, 3:488–492.
Klungel OH, Stricker BHC, Paes AHP, et al.: Excess stroke among hypertensive men and women attributable to undertreatment of hypertension. Stroke 1999, 30:1312–1318.
McCombs JS, Nichol MB, Newman CM, Schlar DA: The costs of interrupting antihypertensive drug therapy in a Medicaid population. Med Care 1994, 32:214–226.
Mar J, Rodriques-Artalejo F: Which is more important for the efficiency of hypertension treatment: hypertension stage, type of drug or therapeutic compliance? J Hypertens 2001, 19:149–155.
Hughes D, McGuire A: The direct costs to the NHS of discontinuing and switching prescriptions for hypertension. J Hum Hypertens 1998, 12:533–537.
Nelson EC, Stason WB, Neutra RB, Solomon HS: Identification of the noncompliant hypertensive patient. Preventive Med 1980, 9:504–517.
Lip GYH, Beevers DG: A survey of the current practice of treating hypertension in primary care: The rational evaluation and choice in hypertension (REACH) study. J Drug Devel Clin Pract 1996, 8:161–169.
Bloom BS: Daily regimen and compliance with treatment [editorial]. BMJ 2001, 323:647.
Borrild NJ: Patients’ experiences of antihypertensive drugs in routine use: Results of a Danish general practice survey. Blood Press 1997, 6(Suppl 1):23–25.
Goldberg AI, Dunlay MC, Sweet CS: Safety and tolerability of losartan potassium, an angiotensin II receptor antagonist, compared with hydrochlorothiazide, atenolol, felodipine ER, and angiotensin-converting enzyme inhibitors for the treatment of systemic hypertension. Am J Cardiol 1995, 75:793–795.
Moore MA, Edelman JM, Gadick LF, et al.: Choice of initial antihypertensive medication may influence the extent to which patients stay on therapy: a community based study of a losartan-based regimen vs. usual care. High Blood Press 1998, 7:156–167.
Grégoire J-P, Moisan J, Guibert R, et al.: Tolerability of antihypertensive drugs in a community-based setting. Clin Ther 2001, 23:715–726.
Jones JK, Gorkin L, Lian JF, et al.: Discontinuation of and changes in treatment after start of new course of antihypertensive drugs: a study of a United Kingdom population. BMJ 1995, 311:293–295.
Monane M, Bohn RL, Gurwitz JH, et al.: Compliance with antihypertensive therapy among elderly Medicaid enrollees: The roles of age, gender, and race. Am J Public Health 1996, 86:1805–1808.
Monane M, Bohn RL, Gurwitz JH, et al.: The effects of initial drug choice and comorbidity on antihypertensive compliance: results from a population-based study in the elderly. Am J Hypertens 1997, 10:697–704.
Rizzo JA, Simons RW: Variations in compliance among hypertensive patients by drug class: implications for health care costs. Clin Ther 1997, 19:1446–1457.
Okano GJ, Rascati KL, Wilson JP, et al.: Patterns of antihypertensive use among patients in the US Department of Defense database initially prescribed an angiotensin-converting enzyme inhibitor or calcium channel blocker. Clin Ther 1997, 19:1433–1445.
Caro JJ, Speckman JL, Salas M, et al.: Effect of initial drug choice on persistence with antihypertensive therapy: the importance of actual practice data. Can Med Assoc J 1999, 160:41–46.
Caro JJ: Stepped care for hypertension: are the assumptions valid? J Hypertens 1997, 15(Suppl 7):S35-S39.
Mann RD, Mackay F, Pearce G, et al.: Losartan: a study of pharmacovigilence data on 14,522 patients. J Hum Hypertens 1999, 13:551–557.
Bloom BS: Continuation of initial antihypertensive medication after 1 year of therapy. Clin Ther 1998, 20:1–11. The first published study (to include an angiotensin II antagonist) on persistence patterns with antihyptertensive medication classes.
Conlin PR, Gerth WC, Fox J, et al.: Four-year persistence patterns among patients initiating therapy with the angiotensin II receptor antagonist losartan versus other antihypertensive drug classes. Clin Ther 2001, 23:1999–2010. This publication is the first to report on persistence patterns over 4 years in patients initiating therapy with the angiotensin II receptor antagonist losartan. The percentage of patients staying on angiotensin II antagonist therapy from 12 months to 48 months was statistically greater (P< 0.001) than the percentage of patients receiving initial therapy with other antihypertensives.
Benson S, Vance-Bryan K, Raddatz J: Time to patient discontinuation of antihypertensive drugs in difference classes. Am J Health Syst Pharm 2000, 57:51–54.
Caro JJ, Salas J, Speckman JL, et al.: Persistence with treatment in hypertension in actual practice. Can Med Assoc J 1999, 160:31–37.
Conlin PR, Fox J, Gerth WC, et al.: Losartan/angiotensin II antagonists have greater persistence than other antihypertensive agents/classes [abstract]. Am J Hypertens 2002, 15(Part 2):29A.
Pham HT, Gause D, Frech FH: Discontinuation, switching and adding among antihypertensive drug classes [abstract]. Am J Hypertens 2001, 14:(Part 2):112A.
Wogen J, Krejilick CA, Livornese RC, et al.: A population-based study of compliance and persistency with cardiovascular agents used in hypertension management [abstract]. Am J Hypertens 2001, 14(Part 2):112A.
Wannemacher AJ, Schepers GP, Townsend KA: Antihypertensive medication compliance in a veterans affairs healthcare system. Ann Pharmacother 2002, 36:986–991.
Marentette MA, Gerth WC, Billings DK, Zarnke KB: Antihypertensive persistence and drug class. Can J Cardiol 2002, 18:649–656.
Chaput AJ: Persistency with angiotensin receptor blockers (ARB) versus other antihypertensives (AHT) using the Saskatchewan Database [abstract]. Can J Cardiol 2000, 16(Suppl F):194F.
Degli Esposti E, Sturani A, Degli Esposti L, et al.: Pharmacoutilization of antihypertensive drugs: a model of analysis. Int J Clin Pharmacol Ther 2001, 39:251–258.
Degli Esposti E, Sturani A, DiMartino M: Long-term persistence with antihypertensive drugs in new patients. J Hypertens 2002, 16:439–444.
Hasford J, Mimran A, Simons WR: A population-based European cohort study of persistence in newly diagnosed hypertensive patients. J Hum Hypertens 2002, 16:569–575.
Mackay FJ, Pearce GL, Mann RD: Cough and angiotensin II inhibitors: cause or confounding? Br J Clin Pharmacol 1998, 46:111–114.
Blood Pressure Lowering Treatment Trialist’ Collaboration: Effects of ACE inhibitors, calcium antagonists, and other blood-pressure lowering drugs: results of prospectively designed overviews of randomized trials. Lancet 2000, 355:1955–1964.
Pitt B, Segal R, Martinez FA, et al.: Randomized trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE). Lancet 1997, 349:747–752.
Pitt B, Poole-Wilson PA, Segal R, et al.: Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomized trial - the Losartan Heart Failure Survival Study ELITE II. Lancet 2000, 355:1582–1587.
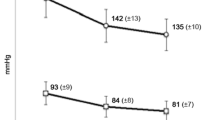
Dahlóf B, Devereux RB, Kjeldsen SE, et al.: Cardiovascular morbidity and mortality in the losartan intervention for endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002, 359:995–1003. The LIFE trial demonstrated a statistically significant 13% reduction in cardiovascular morbidity and mortality clinical endpoints with losartan compared with atenolol. The benefits observed did not appreciably change after adjustment in main outcome for changes in systolic, diastolic, or mean artrial pressure. This study is the first active treatment controlled study in hypertension in which one antihypertensive agent (angiotensin II antagonist, losartan) was superior to an other established antihypertensive agent (β-blocker, atenolol). Discontinuation as a result of all adverse events, drug-related adverse events, and serious drug-related adverse events was significantly less common in losartan-than in atenolol-treated patients.
Brenner BM, Cooper ME, De Zeeuw D, et al.: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001, 345:861–869. In type 2 diabetics with nephropathy, losartan significantly reduced the incidence of doubling of serum creatinine and end-stage renal disease, but had no effect on the rate of death compared with placebo. The benefits observed exceeded those attributable to blood pressure. Both treatment groups received study medication in addition to conventional antihypertensive treatment (calcium channel antagonists, diuretics, α-blockers, β-blockers, and centrally acting agents). More patients discontinued the study treatment in the placebo group (53.5%) than in the losartan group (46.5%).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gerth, W.C. Compliance and persistence with newer antihypertensive agents. Current Science Inc 4, 424–433 (2002). https://doi.org/10.1007/s11906-002-0021-6
Issue Date:
DOI: https://doi.org/10.1007/s11906-002-0021-6