Abstract
BACKGROUND
Screening patterns among primary care physicians (PCPs) may be influenced by patient age and comorbidity. Colorectal cancer (CRC) screening has little benefit among patients with limited life expectancy.
OBJECTIVE
To characterize the extent to which PCPs modify their recommendations for CRC screening based upon patients’ increasing age and/or worsening comorbidity
DESIGN
Cross-sectional, nationally representative survey.
PARTICIPANTS
The study comprised primary care physicians (n = 1,266) including general internal medicine, family practice, and obstetrics-gynecology physicians.
MAIN MEASURES
Physician CRC screening recommendations among patients of varying age and comorbidity were measured based upon clinical vignettes. Independent variables in adjusted models included physician and practice characteristics.
KEY RESULTS
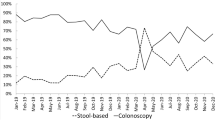
For an 80-year-old patient with unresectable non-small cell lung cancer (NSCLC), 25 % of PCPs recommended CRC screening. For an 80-year-old patient with ischemic cardiomyopathy (New York Heart Association, Class II), 71 % of PCPs recommended CRC screening. PCPs were more likely to recommend fecal occult blood testing than colonoscopy as the preferred screening modality for a healthy 80-year-old, compared to healthy 50- or 65-year-old patients (19 % vs. 5 % vs. 2 % p < 0.001). For an 80-year-old with unresectable NSCLC, PCPs who were an obstetrics-gynecology physician were more likely to recommend CRC screening, while those with a full electronic medical record were less likely to recommend screening.
CONCLUSIONS
PCPs consider comorbidity when screening older patients for CRC and may change the screening modality from colonoscopy to FOBT. However, a sizable proportion of PCPs would recommend screening for patients with advanced cancer who would not benefit. Understanding the mechanisms underlying these patterns will facilitate the design of future medical education and policy interventions to reduce unnecessary care.

Similar content being viewed by others
References
U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–37.
Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58(3):130–60.
Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst. 2010;102(9):605–13.
Klabunde CN, Lanier D, Nadel MR, McLeod C, Yuan G, Vernon SW. Colorectal cancer screening by primary care physicians: recommendations and practices, 2006–2007. Am J Prev Med. 2009;37(1):8–16.
Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283(13):1715–22.
Peabody JW, Luck J, Glassman P, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141(10):771–80.
Cooper GS, Fortinsky RH, Hapke R, Landefeld CS. Primary care physician recommendations for colorectal cancer screening. Patient and practitioner factors. Arch Intern Med. 1997;157(17):1946–50.
Kahi CJ, van Ryn M, Juliar B, Stuart JS. Imperiale TF. Provider Recommendations for Colorectal Cancer Screening in Elderly Veterans. J Gen Intern Med. 2009;18:18.
National Survey of Primary Care Physicians' Recommendations and Practices. Colorectal and Lung Cancer Screening Questionnaire. http://healthservices.cancer.gov/surveys/screening_rp/. Accessed April 9, 2012.
Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997;111(6):1710–7.
Walter LC, Lindquist K, Nugent S, et al. Impact of age and comorbidity on colorectal cancer screening among older veterans. Ann Intern Med. 2009;150(7):465–73.
Hoffman RM, Walter LC. Colorectal cancer screening in the elderly: the need for informed decision making. J Gen Intern Med. 2009;24(12):1336–7.
Schwartz LM, Woloshin S, Fowler FJ Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71–8.
Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic health records and quality of diabetes care. N Engl J Med. 2011;365(9):825–33.
Yabroff KR, Saraiya M, Meissner HI, et al. Specialty differences in primary care physician reports of papanicolaou test screening practices: a national survey, 2006 to 2007. Ann Intern Med. 2009;151(9):602–11.
Cooke M. Cost consciousness in patient care–what is medical education's responsibility? N Engl J Med. 2010;362(14):1253–5.
Walter LC, Davidowitz NP, Heineken PA, Covinsky KE. Pitfalls of converting practice guidelines into quality measures: lessons learned from a VA performance measure. JAMA. 2004;291(20):2466–70.
Mack JW, Wolfe J, Cook EF, Grier HE, Cleary PD, Weeks JC. Hope and prognostic disclosure. J Clin Oncol. 2007;25(35):5636–42.
Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–41.
Hesse BW, Nelson DE, Kreps GL, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165(22):2618–24.
Fisher ES, Berwick DM, Davis K. Achieving health care reform–how physicians can help. N Engl J Med. 2009;360(24):2495–7.
Acknowledgements
Funding support for this study was provided by the National Cancer Institute (contract number N02-PC-51308), the Agency for Healthcare Research and Quality (inter-agency agreement numbers Y3-PC-5019-01 and Y3-PC-5019-02), and the Centers for Disease Control and Prevention (inter-agency agreement number Y3-PC-6017-01). Dr. Haggstrom is the recipient of VA HSR&D Career Development Award CD207016-2.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Cancer Institute, Department of Veterans Affairs, or the Centers for Disease Control and Prevention.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 79 kb)
Rights and permissions
About this article
Cite this article
Haggstrom, D.A., Klabunde, C.N., Smith, J.L. et al. Variation in Primary Care Physicians’ Colorectal Cancer Screening Recommendations by Patient Age and Comorbidity. J GEN INTERN MED 28, 18–24 (2013). https://doi.org/10.1007/s11606-012-2093-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2093-6