Abstract
Background
Disparities in blood pressure (BP) control may be a function of disparities in treatment intensification (TI).
Objective
To examine racial differences in TI, understand modifiable factors that may mediate this relationship, and explore the relative effects of TI and race on blood pressure.
Design
Prospective cohort study.
Participants
Participants were 819 black and white patients with hypertension from an urban, safety-net hospital
Main Measures
We sequentially explored the effects of patient race, sociodemographic and clinical characteristics, beliefs about BP/medications, perceptions of provider/discrimination, sodium intake, medication adherence, and provider counseling on TI, performing a series of random effects analyses. To assess the effects of race and TI on BP, we performed linear regressions, using systolic BP (SBP) as the outcome.
Key Results
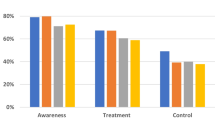
Unadjusted analyses and those including sociodemographic and clinical characteristics revealed that black patients had less TI than whites (−0.31 vs.−0.24, p < 0.001), but adjustment for patient beliefs and experiences eliminated the effects of race (β =−0.02, p = 0.5). Increased patient concerns about BP medications were related to lower TI, as was more provider counseling (β =−0.06, p = 0.02 and β = −0.01, p = 0.001, respectively). In the unadjusted analysis, black race was a significant predictor of SBP (134 mm/Hg for blacks vs. 131 mm/Hg for whites, p = 0.009), but when both race and TI were included in the model, TI was a significant predictor of SBP (final SBP 2.0 mm/Hg lower for each additional therapy increase per 10 visits, p < 0.001), while race was not (Blacks 1.6 mm/Hg higher than whites, p = 0.17).
Conclusions
Improved patient–provider communication targeted towards addressing patient concerns about medications may have the potential to reduce racial disparities in TI and ultimately, BP control.
Similar content being viewed by others
References
Hertz R, Unger A, Cornell J, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104.
Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002.
Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–27.
Nesbitt SD. Hypertension in black patients: special issues and considerations. Curr Hypertens Rep. 2005;7:244–8.
Hajjar I, Kotchen T. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. J Am Med Assoc. 2003;290:199–206.
Chobanian A, Bakris G, Black H, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. J Am Med Assoc. 2003;289:2560–72.
Wong M, Shapiro M, Boscardin W, Ettner S. Contributions of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–92.
Phillips LS, Branch WT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Berlowitz D, Ash AA, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63.
Rose AJ, Shimada SL, Rothendler JA, et al. The accuracy of clinician perceptions of "usual" blood pressure control. J Gen Intern Med. 2007.
Selby JV, Uratsu CS, Fireman B, et al. Treatment intensification and risk factor control: toward more clinically relevant quality measures. Med Care. 2009;47:395–402.
Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47:345–51.
Hicks LS, Fairchild DG, Horng MS, Orav EJ, Bates DW, Ayanian JZ. Determinants of JNC VI guideline adherence, intensity of drug therapy, and blood pressure control by race and ethnicity. Hypertension. 2004;44:429–34.
Safford MM, Halanych JH, Lewis CE, Levine D, Houser S, Howard G. Understanding racial disparities in hypertension control: intensity of hypertension medication treatment in the REGARDS study. Ethn Dis. 2007;17:421–6.
Rose A, Berlowitz D, Manze M, Orner M, Kressin N. Comparing methods of measuring treatment intensification in hypertension care. Circulation Cardiovascular Quality and Outcomes. 2009;2:385–91.
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health. 1999;14:1–24.
Horne R, Buick D, Fischer M, Leake H, Cooper V, Weinman J. Doubts about the necessity and concerns about adverse effects: identifying the types of beliefs that are associated with non-adherence to HAART. Int J STD AIDS. 2004;15:38–44.
Kressin N, Wang F, Long J, et al. Hypertensive patients’ health beliefs, process of care, and medication adherence: is race important? J Gen Intern Med. 2007;22:768–74.
Weinman J, Petrie KJ, Moss-Mossis R, Horne R. The illness perception questionnaire: a new method for assessing the cognitive representation of illness. Psychol Health. 1996;11:431–45.
Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19:101–10.
Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethn Dis. 2001;11:554–63.
Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15:90–6.
Pbert L, Adams A, Quirk M, Hebert J, Ockene J, Luippold R. The patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol. 1999;18:183–8.
Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–86.
Umscheid CA, Gross R, Weiner MG, Hollenbeak CS, Tang SS, Turner BJ. Racial disparities in hypertension control, but not treatment intensification. Am J Hypertens. 2010;23:54–61.
Kerr EA, Zikmund-Fisher BJ, Klamerus ML, Subramanian U, Hogan MM, Hofer TP. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148:717–27.
Ferrari P. Reasons for therapeutic inertia when managing hypertension in clinical practice in non-Western countries. J Hum Hypertens. 2009;23:151–9.
Bokhour B, Long J, Berlowitz D, Kressin N. Assessing patient adherence in medical encounters: How do providers talk with patients about antihypertensive medication taking? J Gen Intern Med. 2006;21:577.
Acknowledgements
The authors thank Mark Glickman, PhD for his advice regarding statistical analyses.
Funding sources
This work was supported by the NIH/National Heart, Lung and Blood Institute grant R01 HL072814 (N. Kressin, PI). Dr. Kressin is supported in part by a Research Career Scientist Award from the Department of Veterans Affairs Health Services Research and Development Service. Dr. Rose is funded by a career development award from the Department of Veterans Affairs Health Services Research and Development Service.
The views expressed in this article are those of the authors and do not necessarily represent the official views and policies of the Department of Veterans Affairs.
Conflict of Interest
None disclosed.
Financial Disclosure
No authors have identified any financial conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manze, M., Rose, A.J., Orner, M.B. et al. Understanding Racial Disparities in Treatment Intensification for Hypertension Management. J GEN INTERN MED 25, 819–825 (2010). https://doi.org/10.1007/s11606-010-1342-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1342-9