Abstract
Background
Optimal warfarin prescription requires correct, individualized assessment of the warfarin-related bleeding risk, which randomised controlled trials may underestimate . Observational studies have reported a range of bleeding risks that differ 40-fold. This variation may be caused by time trends, variation in bleeding definition and study subject selection. We investigated the incidence of, and risk factors for severe bleeding in un-selected warfarin-treated patients from Sweden.
Methods
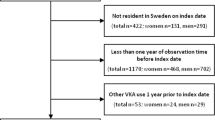
Between 2001 and 2005, 40 centres recruited warfarin-naïve patients commencing warfarin therapy and followed them prospectively with continuous registration of clinical data. The primary outcome was severe bleeding, according to the WHO universal definition of severe adverse drug reactions. The influence of potential risk factors was investigated by means of a Cox proportional-hazards model.
Result
A total of 1523 patients contributed 1276 warfarin-exposed patient-years. The incidence of first-time severe bleeding was 2.3 per 100 patient-years (95% confidence interval 1.4 to 3.1). Male sex and use of drugs potentially interacting with warfarin were the only independent risk factors of severe bleeding, with hazard ratios of 2.8 and 2.3, respectively. Age, target International Normalized Ratio (INR), time spent outside target INR range, and warfarin dose requirement were not significantly associated with bleeding risk.
Conclusions
The risk of severe bleeding in a large naturalistic, prospective cohort of first-time warfarin users was lower than reported in some previous reports. Male gender was an independent predictor of severe bleeding as was the receipt of warfarin-interacting medications at the onset of anticoagulation therapy. Further studies are required to evaluate the effect these findings may have on the quality of current risk-benefit analysis involved in warfarin prescription.


Similar content being viewed by others
References
Linkins LA, Choi PT, Douketis JD (2003) Clinical impact of bleeding in patients taking oral anticoagulant therapy for venous thromboembolism: a meta-analysis. Ann Intern Med 139:893–900
Levine MN, Raskob G, Beyth RJ, Kearon C, Schulman S (2004) Hemorrhagic complications of anticoagulant treatment: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126:287S–310S
Bullano MF, Willey V, Hauch O, Wygant G, Spyropoulos AC, Hoffman L (2005) Longitudinal evaluation of health plan cost per venous thromboembolism or bleed event in patients with a prior venous thromboembolism event during hospitalization. J Manag Care Pharm 11:663–673
Lindh JD, Kublickas M, Westgren M, Rane A (2004) Internet based clinical trial protocols – as applied to a study of warfarin pharmacogenetics. Br J Clin Pharmacol 58:482–487
Läkemedelsindustriföreningen LIF (2003) Fass 2003 (The Swedish catalogue of approved medical products). Stockholm 1710–1712
Beyth RJ, Quinn L, Landefeld CS (2000) A multicomponent intervention to prevent major bleeding complications in older patients receiving warfarin. A randomized, controlled trial. Ann Intern Med 133:687–695
Landefeld CS, Goldman L (1989) Major bleeding in outpatients treated with warfarin: incidence and prediction by factors known at the start of outpatient therapy. Am J Med 87:144–152
Petty GW, Lennihan L, Mohr JP, Hauser WA, Weitz J, Owen J et al (1988) Complications of long-term anticoagulation. Ann Neurol 23:570–574
Bussey HI, Rospond RM, Quandt CM, Clark GM (1989) The safety and effectiveness of long-term warfarin therapy in an anticoagulation clinic. Pharmacotherapy 9(4):214–219
Fihn SD, McDonell M, Martin D, Henikoff J, Vermes D, Kent D et al (1993) Risk factors for complications of chronic anticoagulation. A multicenter study. Warfarin Optimized Outpatient Follow-up Study Group. Ann Intern Med 118:511–520
Beyth RJ, Quinn LM, Landefeld CS (1998) Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin. Am J Med 105:91–99
McMahan DA, Smith DM, Carey MA, Zhou XH (1998) Risk of major hemorrhage for outpatients treated with warfarin. J Gen Intern Med 13:311–316
Chiquette E, Amato MG, Bussey HI (1998) Comparison of an anticoagulation clinic with usual medical care: anticoagulation control, patient outcomes, and health care costs. Arch Intern Med 158:1641–1647
Njaastad AM, Abildgaard U, Lassen JF (2006) Gains and losses of warfarin therapy as performed in an anticoagulation clinic. J Intern Med 259:296–304
Torn M, Bollen WL, van der Meer FJ, van der Wall EE, Rosendaal FR (2005) Risks of oral anticoagulant therapy with increasing age. Arch Intern Med 165:1527–1532
Taghavi A, Jonson T, Stockelberg D (1999) [Survey of complications following treatment with anticoagulants. A computerized search for hemorrhagic complications completes manual reporting] Läkartidningen 96:3421–3424
Witt DM, Sadler MA, Shanahan RL, Mazzoli G, Tillman DJ (2005) Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest 127:1515–1522
Wändell PE (2001) Anticoagulant treatment of patients in Swedish primary health care. Safety aspects. Eur J Clin Pharmacol 57:61–64
Fanikos J, Grasso-Correnti N, Shah R, Kucher N, Goldhaber SZ (2005) Major bleeding complications in a specialized anticoagulation service. Am J Cardiol 96:595–598
Palareti G, Leali N, Coccheri S, Poggi M, Manotti C, D’Angelo A et al (1996) Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet 348:423–428
Petitti DB, Strom BL, Melmon KL (1989) Prothrombin time ratio and other factors associated with bleeding in patients treated with warfarin. J Clin Epidemiol 42:759–764
White RH, Beyth RJ, Zhou H, Romano PS (1999) Major bleeding after hospitalization for deep-venous thrombosis. Am J Med 107:414–424
Oden A, Fahlen M (2002) Oral anticoagulation and risk of death: a medical record linkage study. BMJ 325:1073–1075
Aithal GP, Day CP, Kesteven PJ, Daly AK (1999) Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet 353:717–719
Higashi MK, Veenstra DL, Kondo LM, Wittkowsky AK, Srinouanprachanh SL, Farin FM et al (2002) Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 287:1690–1698
Lindh JD, Lundgren S, Holm L, Alfredsson L, Rane A (2005) Several-fold increase in risk of overanticoagulation by CYP2C9 mutations. Clin Pharmacol Ther 78:540–550
Scordo MG, Pengo V, Spina E, Dahl ML, Gusella M, Padrini R (2002) Influence of CYP2C9 and CYP2C19 genetic polymorphisms on warfarin maintenance dose and metabolic clearance. Clin Pharmacol Ther 72:702–710
D’Andrea G, D’Ambrosio RL, Di Perna P, Chetta M, Santacroce R, Brancaccio V et al (2005) A polymorphism in the VKORC1 gene is associated with an interindividual variability in the dose-anticoagulant effect of warfarin. Blood 105:645–649
Vecsler M, Loebstein R, Almog S, Kurnik D, Goldman B, Halkin H et al (2006) Combined genetic profiles of components and regulators of the vitamin K-dependent gamma-carboxylation system affect individual sensitivity to warfarin. Thromb Haemost 95:205–211
Veenstra DL, You JH, Rieder MJ, Farin FM, Wilkerson HW, Blough DK et al (2005) Association of Vitamin K epoxide reductase complex 1 (VKORC1) variants with warfarin dose in a Hong Kong Chinese patient population. Pharmacogenet Genomics 15:687–691
Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, Eriksson N et al (2005) Common VKORC1 and GGCX polymorphisms associated with warfarin dose. Pharmacogenomics J 5:262–270
Acknowledgments
Jonatan D. Lindh is supported by the Swedish Foundation for Strategic Research. The project was supported by the Swedish Science Council (Medicine 04496), Nycomed AB, and the Swedish Drugs and Therapeutics Committee of Southwest Stockholm.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindh, J.D., Holm, L., Dahl, ML. et al. Incidence and predictors of severe bleeding during warfarin treatment. J Thromb Thrombolysis 25, 151–159 (2008). https://doi.org/10.1007/s11239-007-0048-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-007-0048-2